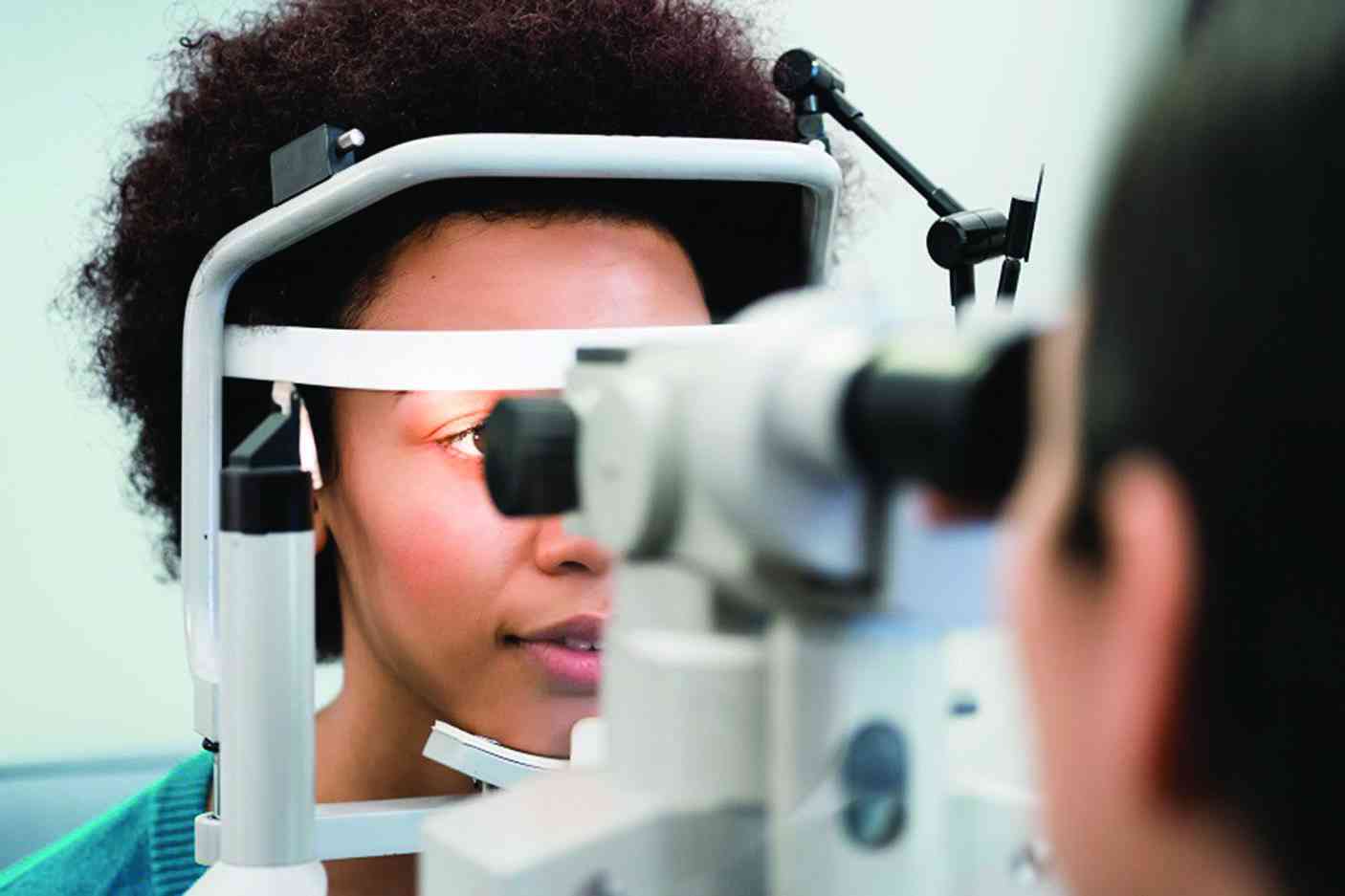
VISION is the most dominant of our senses, which supports independence and functionality, and yet very little attention is given when a person experiences poor vision because it is not considered life-threatening.
Poor vision affects daily living, work performance and ultimately the quality of life. Cataract causes cloudiness in the lens of the eye resulting in blurred vision.
Ageing is the primary risk of cataract influenced by ultraviolet exposure, smoking and poor nutrition, among other factors.
According to the World Report on Vision (2019), globally 65,2 million people have a vision impairment due to cataract.
Cataract is the leading cause of avoidable blindness in the world and in Zimbabwe.
According to the results of Rapid Assessment of Avoidable Blindness (RAAB) conducted in Manicaland (2016), Masvingo (2019) and Matabeleland South provinces (2019) an estimated average of 65% of people aged 50 years and above suffer from untreated cataract indicating a huge burden that requires collaborative efforts.
However, the burden is not equitable as it varies by age, gender, location and income level. The treatment for cataract is a surgical intervention that removes the opaque lens of the eye and replaces it with an artificial ocular lens.
This is usually done using manual small incision procedure which is considered cost effective or phacoemulsification. It should be noted that after successful cataract surgery, a patient is able to carry out their daily tasks with ease.
- Nurses fume over paltry govt loans
- 'Apostolic sects frustrating fight against measles'
- Opinion: GZU School of Medicine should improve health service in Masvingo
- Mpilo doctors’ quarters rehab complete
Keep Reading
When corneal blindness decreases due to management of measles and vitamin A deficiency, cataracts are also common in children.
A number of people live with vision impairment or blindness that can be prevented because they are not aware of the condition and the services available.
Generally, access to eye care services is influenced by availability of service, accessibility, affordability and acceptability.
Barriers to accessing services
The cost of cataract surgery is still high and without health insurance the majority cannot afford. Even in cases where the services are subsidised, the patient out of pocket payments which include transport and accommodation, discourage the patient from seeking eye care services.
Using the goat index a person residing in the rural areas may need to sell four goats in order to access cataract services. Fear is another barrier that hinders access because people are afraid of the procedure due to sensitivity of the eye and subsequent eye health outcomes.
Poverty and competing priorities have influenced access to eye care services in general. Eye health conditions are not prioritised as a result a person can decide to weigh the opportunity costs and opt for basic needs such as food instead of cataract surgery.
There is inequitable distribution of the current eye care work force, which is not addressing the population needs. Most of the services are provided at secondary and tertiary level further exacerbating inequity in access.
In some cases, the equipment required to provide the services is not available. A number of studies indicate that women do not have the same access to services as men and a less likely to undergo cataract surgery.
Gender inequity is influenced by a number of socio economic and cultural factors. People who have other forms of disabilities have struggled to access eye care services compared to people without disabilities.
For example, a person with hearing impairment or learning disabilities would require additional support and inclusive services. It has been noted that a number of people did not access cataract services because they were not aware of the eye condition or services available.
Culture has influenced access to eye care services as people have resorted to traditional harmful practices, such as the use of milk or urine.
Recommendations
Health promotion interventions are essential in promoting the uptake of cataract services and addressing unhealthy behaviours. Through health promotion people are empowered to make choices and made aware of the eye condition.
Higher levels of patient engagement are necessary in order to understand their needs, concerns and offer services that are appropriate.
For example, a patient may want to know how to access support post-surgery at a nearby health facility. The best advocate for cataract services is someone who has undergone cataract surgery.
It is, therefore, imperative that the quality of services and outcomes is good to ensure that more people come for cataract surgery. The quality and outcome of cataract surgery should be monitored systematically and reported as per the good vision outcome threshold.
While monitoring the quantity (cataract surgical coverage) is important in addressing the backlog, measuring the quality (effective cataract surgical coverage) of surgery at base hospital and outreach cannot be compromised. Even in cases where sight cannot be restored due to other underlying conditions, the patient should be made aware and provided with the necessary rehabilitation support.
The country has been affected by the effects of the brain drain where a number of trained eye health personnel have left the country for greener pastures, thus affecting the availability of eye care services.
An investment should be made to train additional human resources for eye health in order to address the need.
The Ministry of Health and Child Care, in collaboration with partners, should ensure the provision of equipment, consumables and drugs to enable affordable quality cataract services.
Where possible, services should be subsidised to increase access and at the same time put measures in place to promote sustainability.
Outreach services are important for making cataract services more accessible, especially for the under-served communities. In addition, outreach services reduce the patient out of pocket payments.
However, it is important that quality is maintained when services are provided on outreach and a clear plan for post operative review established.
Post-operative visual acuity has to be measured at two weeks and six weeks after surgery, but at times the patients do not return for review because of the cost of travelling.
This is an opportunity for the private sector, local companies to partner and support the cost of surgery for patients who cannot afford. Private sector support can include, volunteering, sponsoring the surgery through the provision of consumables.
The integration of primary eye care into primary health care will enhance the identification, referral and treatment of cataract patients. The establishment of high-volume cataract centres will assist in reducing the cataract surgical backlog.
A team-based approach is required to increase cataract surgery output. This will entail bulk procurement of surgical consumables, efficient use of time for theatre staff with the aim of reducing the costs per patient and offering affordable services.
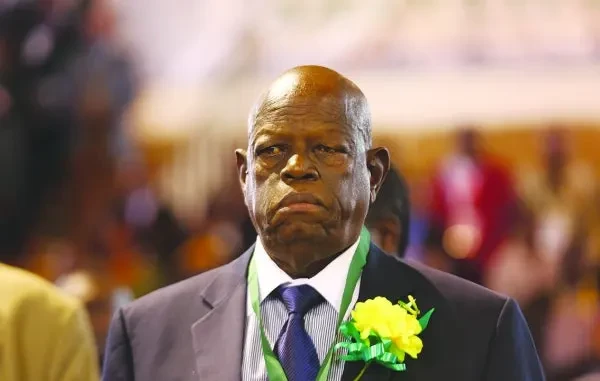
- Tigere is a development practitioner and writes in her personal capacity. These weekly New Horizon articles, published in the Zimbabwe Independent, are co-ordinated by Lovemore Kadenge, an independent consultant, managing consultant of Zawale Consultants (Pvt) Ltd, past president of the Zimbabwe Economics Society and past president of the Chartered Governance & Accountancy Institute in Zimbabwe (CGI Zimbabwe). — [email protected] or +263 772 382 852.