Village health worker Lizzy Siziba of Mberengwa wipes sweat from her brow after walking nearly five kilometres.
Then, she shares a light moment with Siduduzile Moyo, whose child, once malnourished, has recovered after a visit to a clinic and three months on Plumpy’Nut.
With her mid-upper arm circumference (MUAC) tape in one hand and her register in the other, Siziba’s feet may be tired, but her smile is unwavering as she steps into a homestead she knows well.
There is mutual respect for the 62-year-old who has been doing this work since 2001. She goes straight into the business of the day.
She asked: “How has the child been since the last time we saw each other, and what have you been feeding her?”
Siziba listened attentively as she was told the child is doing well.
She had been told to stop the Plumpy Nut at the health facility to which she was referred.
But Siziba paused when she was told that the child is fed porridge and sadza, a staple food in Zimbabwe, typically consisting of just maize and water, which does not provide enough nutrients for a growing child.
- NGO ‘builds bridges’ in Mberengwa
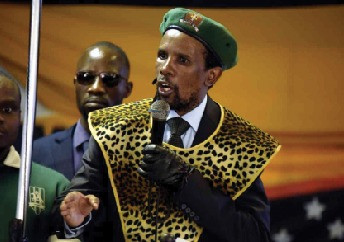
- Vote Zanu PF, chief tells villagers
- Mberengwa clinic gets tap water
- Clash over vendors, youths welfare
Keep Reading
In this case, the village health work realised the mother was struggling to meet the recommended diet for her child as previously advised.
In Zimbabwe, Plumpy'Nut is a vital, peanut-based paste used to treat children suffering from severe acute malnutrition (SAM). It is known as a ready-to-use therapeutic food (RUTF).
It is enriched with essential vitamins and minerals, providing a high-energy, medical food supplement that doesn't require refrigeration or preparation.
The village health worker asked, “What about our four-star diet?”
This question reminded Moyo that despite the child's good performance, she had not followed some advice.
In Zimbabwe, the four-star diet is a simple guide to help families fight malnutrition, especially in children. It encourages eating a mix of foods from four critical groups: animal foods like meat or eggs, staple foods like sadza or rice, legumes like beans, and colourful fruits and vegetables. This diet is part of the country’s plan to ensure children grow healthy and strong.
As Siziba wrapped the MUAC tape around the child’s arm, the indicator fell in the yellow zone, signalling moderate acute malnutrition.
This is a setback, as the child had previously recovered and been weaned off Plumpy’Nut.
The yellow section on a MUAC tape indicates that a child is at risk of malnutrition. This means the child is not yet severely malnourished (which would fall in the red zone), but she requires close monitoring, extra attention at mealtimes at home, and follow-up to prevent her condition from worsening.
“This is why regular visits are so important,” Siziba said.
“As a village health worker, I know that raising awareness isn’t something you do just once.
“We must keep returning to our communities to remind mothers and caregivers that our support for children must continue.
“This child may have been overlooked simply because after the clinic said she was doing well, we assumed we could shift our focus to other villages.”
The role of village health workers in Zimbabwe’s health sector cannot be overstated.
Operating at the primary level, they focus on disease prevention and community care, particularly in rural and peri-urban wards.
These dedicated workers serve as a bridge between communities and the formal health system.
Village health workers like Siziba have seen it all. Mberengwa is considered drought-prone, hence the importance of their work for children’s health.
When drought strikes, the land hardens, harvests shrink, and livestock perish.
For families in rural Zimbabwe, it means plates with less food and fewer choices. And often, it’s the youngest who suffer first.
In the last El Niño-induced drought of 2015–2016, Zimbabwe saw a 25% spike in the number of children needing treatment for severe acute malnutrition.
The warning signs were clear. So this time, with another harsh El Niño looming, communities and partners acted early.
From village paths to national boardrooms, people came together.
Care groups and village health Workers intensified their efforts on the ground—visiting homes, educating mothers, and monitoring children’s growth. They weren’t alone.
Agricultural partners worked hand in hand with health and nutrition teams.
Community nutrition gardens were set up near water sources, and families learned to grow more resilient crops.
Caregivers were trained to prepare nutritious porridge for young children, enriched with multiple micronutrient powders.
With support from the Health Resilience Fund (HRF) comprising the European Union, the governments of Ireland and the United Kingdom, and Gavi, the Vaccine Alliance, and with the Central Emergency Response Fund (CERF), Unicefcand partners worked alongside the Ministry of Health and Child Care to expand MUAC screening across high priority districts, ensuring no child’s condition went unnoticed.
The results were telling. In districts where care groups were active and different sectors worked together, children’s nutrition status remained stable, even after the drought.
Brighton Makumbe, the district nutritionist for Mberengwa, commended Unicef and the Health Resilience Fund (HRF) funding, which has made a tangible difference in the community.
“We trained our village health workers in malnutrition screening to support early detection of cases,” Makumbe said.
“This enables us to make timely, data-driven decisions, including distributing nutrition commodities such as Plumpy’Nut.”
He explained that reaching vulnerable communities was far more difficult because proper mapping was not used to identify areas with the most urgent needs.
“Nurses and other health professionals are involved in the work carried out by village health workers and traditional leaders like chiefs,” Makumbe said.
“Their efforts are helping save the lives of many children.”
Kosam Sibanda, the nurse-in-charge at Mwanezi Clinic in Mberengwa, echoed his sentiments.
“We have eight trained village health workers who use MUAC tapes to screen for malnutrition,” Sibanda said.
“A study showed a spike in cases, largely due to the prolonged drought.
“The children were referred to us, and we conducted rescreening before initiating them on RUTF) like Plumpy’Nut.
“Without these trained VHWs, many of these children would never have reached us. It has truly been lifesaving.”
As Siziba left Moyo’s homestead, she remarked: “Someone must walk these kilometres so that a child can become a community leader, a doctor, or a teacher.
“That is what keeps me and others going.”
— Unicef