Schools are not only centres of learning but also critical environments for shaping the health and wellbeing of children and adolescents.
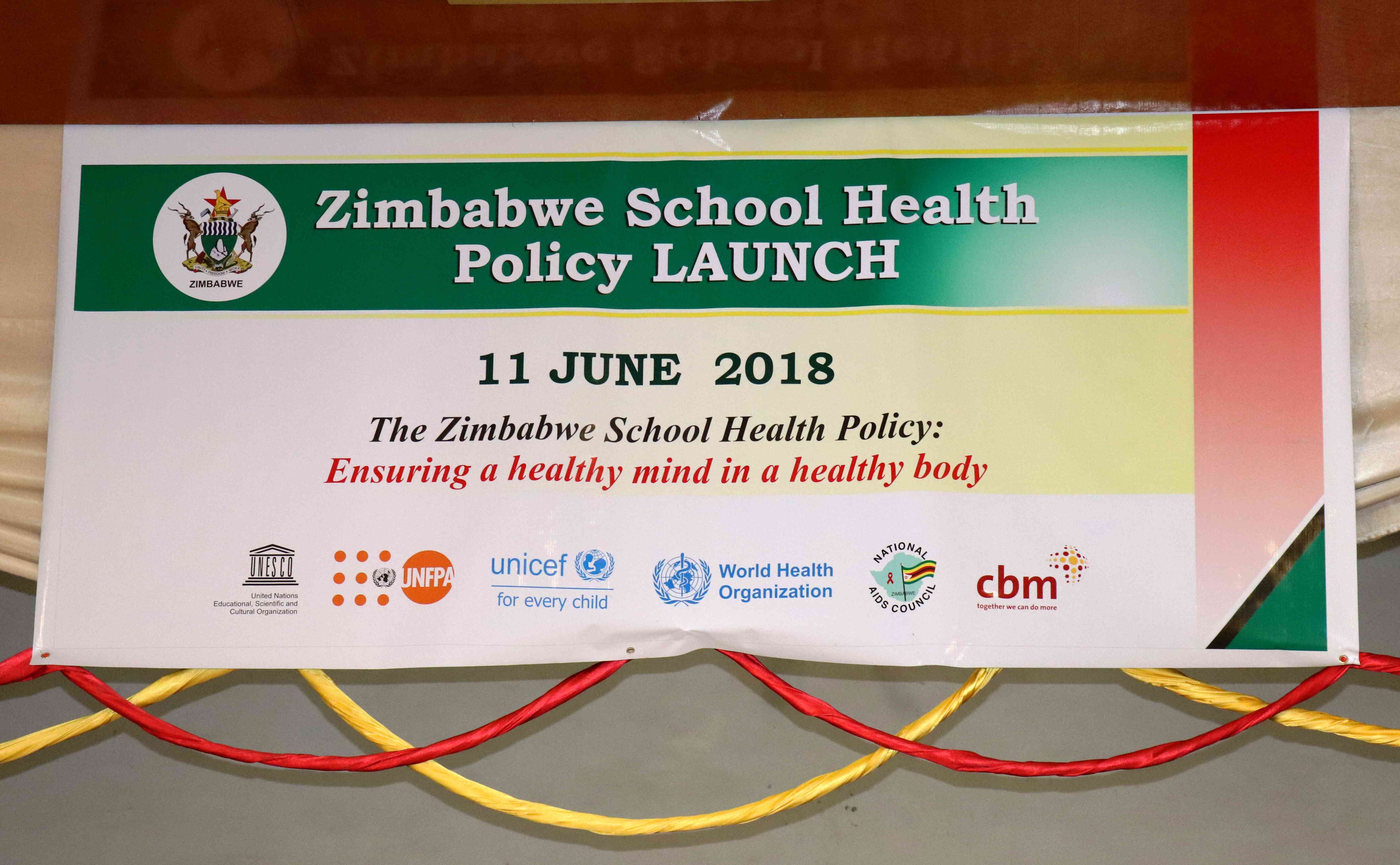
They are safe havens and safety nets for children. In recognition of this, the Government of Zimbabwe adopted the School Health Policy (2018) as a framework to promote learner health, enhance educational outcomes, and safeguard children’s rights.
The policy adopts a holistic approach, addressing nutrition, sexual and reproductive health, mental health, water and sanitation, and child protection.
The Zimbabwe School Health Policy (ZSHP) emanates from the recognition of the inseparable relationship between education and health and the fact that many ailments can be prevented through appropriate interventions at the earliest stages of human life (Zimbabwe School Health Policy,2018).
Looking from a community psychology perspective, the policy reflects efforts to empower learners, families, and communities while fostering intersectoral collaboration for systemic change.
This review highlights the strengths of the School Health Policy, identifies gaps and challenges, and offers recommendations for strengthening its implementation.
One of the notable strengths of the Zimbabwe School Health Policy is its holistic and comprehensive design.
It recognises that learner wellbeing extends beyond physical health to include psychosocial support, safety, and the acquisition of life skills.
- Teachers, other civil servants face off
- Veld fire management strategies for 2022
- Magistrate in court for abuse of power
- Vungu Dam water treatment and irrigation project takes off
Keep Reading
This multidimensional focus is consistent with international standards such as the WHO’s Global School Health Initiative.
The policy is also firmly rooted in a rights-based and inclusive approach. Anchored in the Constitution of Zimbabwe and various international conventions, it upholds learners’ rights to both health and education.
By prioritising vulnerable groups such as girls, children with disabilities, orphans, and by being gender sensitive it makes an important step toward equity and social justice.
Another strength lies in its emphasis on multi-sectoral collaboration. The policy promotes coordination between Ministry of Health and Child Care and Ministry of Primary and Secondary Education, and other government ministries while also encouraging partnerships with NGOs and communities.
This opens space for collective action, integrated service delivery and resource sharing. Its preventive and promotive orientation further enhances its relevance, as it emphasizes life skills, immunisation, awareness campaigns and other interventions that shift attention from treatment to prevention.
The policy’s integration within the education system also makes health interventions more accessible and sustainable, ensuring that children’s health supports their learning outcomes.
Equally important is its explicit focus on child protection and psychosocial support, which strengthens mechanisms to prevent violence, bullying, and abuse while promoting referral pathways for learners in distress.
The alignment of the policy with global and national agendas, including the Sustainable Development Goals and Zimbabwe’s national development strategies, reinforces its legitimacy and vision.
Lastly, the encouragement of community participation, particularly through school leadership, parents, and learners themselves, enhances sustainability by strengthening local ownership.
Despite these strengths, the policy faces several challenges that undermine its effectiveness.
Implementation capacity remains limited, with many schools lacking trained health coordinators, nurses, or counsellors to translate policy into action.
This has led to uneven progress across different regions, particularly disadvantaging rural and resource-constrained schools.
Child protection enforcement remains inconsistent, with reports of sexual abuse, corporal punishment, and bullying persisting despite clear policy provisions.
Weak reporting mechanisms and referral systems leave many cases unaddressed. The fear of victimisation by school personnel assigned to provide psychosocial support to learners calls for unity and community action.
Child protection mechanisms should be strengthened through robust enforcement, safe and confidential reporting pathways, and survivor-centred support services.
Communities must work together with schools to provide a safe environment that safely addresses issues of violence against children.
There is need to put measures that are community based by ensuring community leaders are involved in protecting victims and service providers
Funding is another major constraint, the policy is heavily dependent on donor support, while government allocations remain minimal.
According to the 2025 National Budget produced in in November 2024 the government allocation for health is 13% which is not enough to cover both schools and hospitals with external funding drying up.
To strengthen the School Health Policy, there is need for increased domestic funding to ensure sustainability and continuity of policy implementation despite discontinued or funding cuts by external partners.
Communities can be funders of their own jurisdictions by actively mobilising resources from community members, local business people, private sector and doing school community income generating projects collectively.
In some communities those in the diaspora are already supporting their local community school development projects.
Strengthening relationships with school leavers who have transitioned to employment whether locally or internationally and involving them in planning and implementation of programmes is key for resource mobilisation.
Therefore, to create sustainable funding, funding must start in the community.
Communities will eventually realise that funding does not only encompass money, but can also include community assets, unused land and other resources that can prove to be useful to support community school development.
Community psychologists are there to support asset mapping in the community, help communities realise their potential and ensure community initiatives are successfully implemented.
Weak monitoring and evaluation systems further complicate implementation. Inconsistent tracking of learner health indicators across schools limits accountability and makes it difficult to assess outcomes.
Monitoring and evaluation frameworks must also be reinforced, with clear indicators to track health, psychosocial wellbeing, and child protection outcomes across schools. Monitoring of the policy implementation must be community led.
A community led monitoring team comprising of school and community leadership, learners, parents, health workers and health facility staff must be at the forefront of ensuring the School Health Policy is implemented following guidelines and health outcomes are monitored.
The district and provincial offices may provide technical support and build capacity to these community led committees.
The Ministry of Primary and Secondary Education has done a great job in establishing the Learner Welfare, Psychological Services and Special Needs Education department.
The Department has Psychologists which identify and support learners with disabilities, conducts assessments and support inclusive education initiatives.
However, there is an inadequate number of psychologists based at the provincial office with limited resources to reach out to districts schools especially in rural areas.
The deployment of more specialised personnel, including school nurses and school counsellors is essential, particularly in rural schools where services are most limited.
Expanding the School Psychological Services to district and school level is key for widespread impact, decentralisation of services whilst lessening the burden for provincial psychologists.
The integration of health education into the curriculum and teacher training remains partial.
While life skills and SRHR are mentioned, they are not fully embedded in the curriculum, and most teachers lack adequate preparation to deliver psychosocial support or address sensitive health issues.
Mental health support is particularly underdeveloped, with very few specialized staff housed at provincial level despite the policy’s recognition of psychosocial needs.
Health education must also be fully mainstreamed into the curriculum, accompanied by comprehensive teacher training in SRHR, psychosocial support, psychological first aid, trauma informed care and mental health literacy for effective implementation
Learner and community engagement is also less robust than envisioned. Parents and School Development Committees are not always actively involved in health-related decisions, while learners’ voices are seldom centred in program design and monitoring.
The policy stipulates that its success is heavily dependent on effective coordination, implementation linkages, learner participation, community participation and ownership, monitoring and evaluation.
Learners and communities should be more actively engaged through participatory approaches that empower them to shape priorities, monitor progress, and co-own interventions.
This can be done through establishing mental health awareness campaigns and peer support groups involving learners, parents, and traditional leaders and also incorporating indigenous knowledge systems and community healing practices into school health programs
In summary the Zimbabwe School Health Policy represents a progressive step toward improving the health and educational outcomes of children. Its inclusive and holistic approach is commendable, as is its emphasis on prevention, rights, and community involvement.
However, its impact is constrained by weak implementation capacity, limited funding, inadequate monitoring, and persistent inequalities.
By addressing these gaps through stronger investment, accountability, and community engagement, Zimbabwe can transform its schools into true environments of learning, growth, and wellbeing.
From a community psychology perspective, the policy offers fertile ground for empowering learners and communities, but it must be supported with concrete action to ensure that children thrive in both health and dignity.
*Ottilia Mabhena is an intern community psychologist based at Bulawayo Dominican Convent Schools and affiliated with Identity Consultancy, she writes in her own capacity. She can be contacted on [email protected]